
Positive-pressure ventilation (PPV) is the underlying mechanism of modern mechanical ventilators Once patients show sufficient spontaneous breathing, they are weaned off ventilation support. A systematic approach to common problems in mechanical ventilation (e.g., sudden deterioration, problems with oxygenation and ventilation, hemodynamic compromise, patient-ventilator dyssynchrony, dynamic hyperinflation) is recommended to prevent morbidity and mortality.
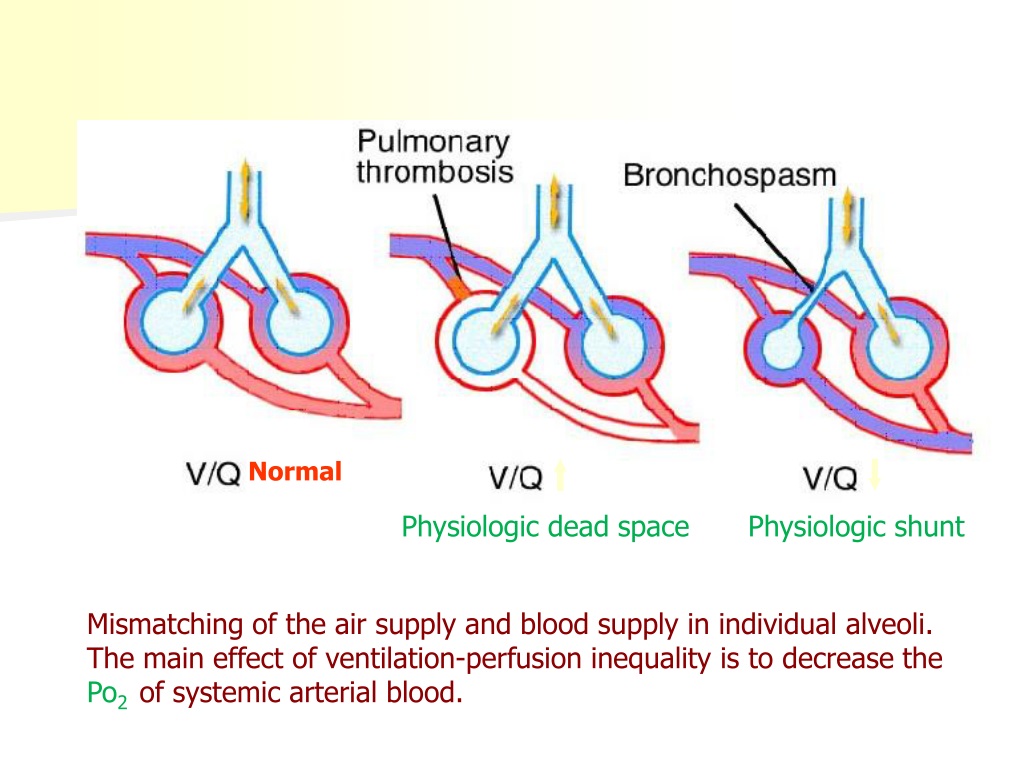
Complications of mechanical ventilation include ventilator-induced lung injury and ventilator-associated pneumonia, as well as extrapulmonary complications such as GI ulcers and venous thromboembolism. These should be implemented in a critical care setting with close monitoring in collaboration with specialists, nurses, and respiratory therapists. A variety of ventilation strategies have been described for treating different types of respiratory failure. Settings such as ventilation modes (e.g., assist-control, pressure-support) and parameters (e.g., tidal volume, respiratory rate, FiO 2, PEEP) should be adjusted to patient needs in order to minimize complications and restore homeostasis. Indications include hypoxemic and hypercapnic respiratory failure, hemodynamic compromise, and the need for close ventilatory control (e.g., therapeutic hyperventilation).

It involves the application of positive pressure, which can be invasive (i.e., in intubated patients) or noninvasive (e.g., CPAP or BiPAP).
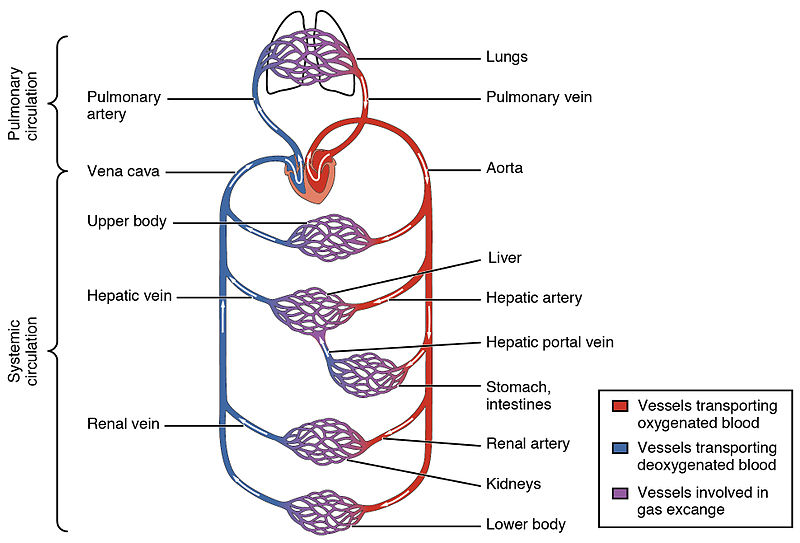
Mechanical ventilation is used to assist or replace spontaneous breathing to reduce the work of breathing and/or reverse life-threatening respiratory derangement in critically ill patients or to maintain respiratory function in those undergoing general anesthesia.


 0 kommentar(er)
0 kommentar(er)
